Surgical Treatment of Hernias on the Anterior Abdominal Wall (inc Paraumbilical, Epigastric) & Incisional Hernias
Surgical options include:
1. Direct repair without mesh – this involves using suturing the defect with nondissolvable sutures eg 1 Nylon. This alone has a higher risk of recurrence. In the past, a Mayo repair is used – this involves overlapping two layers of tissue and suturing the defect together under tension. Again this has a higher risk of recurrence.
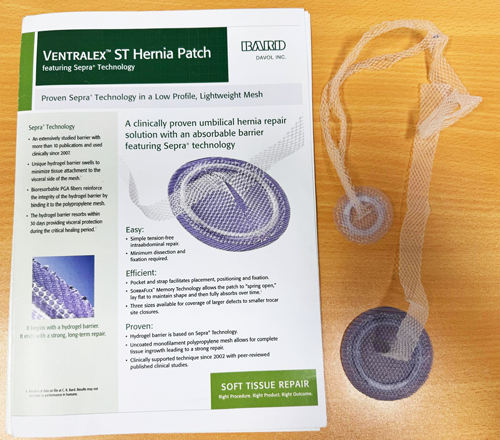
2. Mesh hernioplasty – there are many types of mesh and different techniques - onlay and sublay; open and laparoscopic
TENSION FREE REPAIR WITH Sublay MESH via MINI-INCISION
Dr LP Cheah's preference is to use a sublay Ventralex mesh using only SHORT SINGLE incision. Usually around 2cm.
No muscle paralysis is needed during the anaesthesia so this can be done under local anaesthesia & sedation too(with laparoscopic surgery "keyhole" - muscle paralysis is needed and 3 incisions need to be made elsewhere - this increases the risk of port site hernias)
This mesh is a dual surface mesh with PTFE(smooth) on one side(the side facing the bowel) and polypropelene on the outside.
This is placed in a sublay position – that is under the hole of the hernia defect within the peritoneal cavity(this is much stronger than in an onlay position). The PTFE surface is in contact with the bowel – because this is smooth there is much reduced risk of developing adhesions of the bowel(adhesions can cause small bowel obstruction). The outside surface is the usual polypropelene mesh – the most commonly used mesh. This mesh allows fibrous tissue to grow it. This mesh is secured by suturing its two polypropelene straps to the edges of the hernia defects without any tension. Additional sutures may be used to approximate the gap. The overlying skin is then closed in layers with dissolvable sutures.

Photo: Repair with sublay Ventralex mesh using a short 2cm incision.
Postoperative Care
1. This surgery is usually carried out as a day case for a small hernia
2. It is important to take regular analgesics as soon as one wakes up from the surgery before feeling any pain(ie before the local anaesthesia wears off)
3. Leave the plastic waterproof dressing on for 2 weeks if possible(there is also often a piece of gauze rolled into a ball under that – this is to push the belly button back in and avoid fluid filling the space of the hernia) . Leave the tape dressings(Steristrips) on for a further 1-2 weeks.
4. Surgical review is at 6 to 8 weeks
When to return to driving ? This varies from person to person – the answer is : Firstly check with your car insurance company. Then only drive when one is comfortable especially to apply the brakes! Please discuss this with your doctor.
Click Here To View The Hernia Recovery Timetable
When to return to work?
Because this mesh is placed in a sublay position(ie the mesh to patch the hole from the hernia is placed on the inside of the hernia defect), there is no strict restrictions to be completely off work.
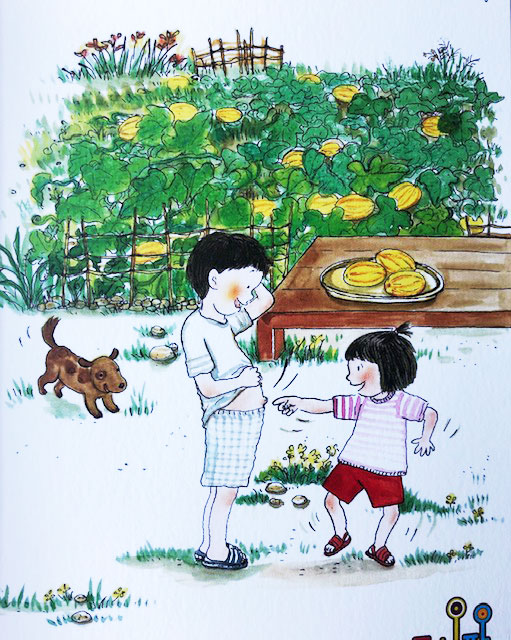
Dr LP Cheah has had patients returning to work within a few days. For example, the next day for office work. A fruiterer, return to his work within 3 days – lifting dozens of boxes of fruits. Some patients choose to take 2-3 weeks off work.
It really depends on how comfortable ones feel from the cut on the skin and the stitches holding the mesh! Dr LP Cheah tries his best in the surgery to minimize the postop pain by:
1. Using as little tension as possible in suturing
2. Minimizing tissue damage and dissection - being efficient here also means shorter anaesthetic time and less risks
3. Keeping the skin scar short and vertical - the incision is usually just a little longer than a keyhole(hence there is no advantage for laparoscopic surgery here)
4. Ensuring a good local anaesthetic block
When can I play golf again? I would advise to start slowly - with putting and chipping. Then gradually do the drives - do not try to hit a hole in one too soon after the surgery !
Risks of surgery
- Risks of anaesthesia
- Scar
- Pain – rarely complex regional pain syndrome
- Bleeding, bruising
- Recurrence – especially from a sutured repair
- Swelling under scar - less with vertical scar
- Adhesions – rarely bowel obstruction(much less with the dual surface mesh)
- Risk from the mesh – the PTFE and polypropelene material are generally inert. Of course with any foreign material placed within the body, new discoveries may be made in future of potential new side-effects. Future laparoscopic surgery may be more difficult – especially if port has to be place around the belly button area! There might also be increased risks of bleeding and of damaging other organs. If there is infection elsewhere in the body especially in the overlying skin(eg folliculitis) - the mesh can potentially get infected. Hence it is important to see your doctor in future if the umbilicus is red or painful. Sometimes the sutures from the mesh can end up sitting just under the skin especially in a thin person - that can be removed at a later stage once the mesh has incorporated if it is bothering the patient.
Mr LP Cheah is an expert in repairing small hernias on the anterior abdominal wall using short incisions. He has learned his techniques from a number of teachers from Britain, Australia and Canada including Mr Maurice Brygel (Melbourne Hernia Clinic) and Mr David Fossard (England).His Ventralex hernia repair technique has been modified to use shorter incisions without needing any laparoscopic surgery(1 short cut instead of 3, no need for muscle relaxants, no risk of port site hernias)